Abstract
Background: The incidence of Venous thromboembolism (VTE) is increasing in the pediatric population which has led to a significant impact on morbidity, mortality and health care costs. The majority of VTE episodes diagnosed in children are considered provoked events secondary to an identifiable risk factor. In contrast, truly unprovoked VTE events are rare in children and there is limited data describing clinical course and outcomes in this population. The aim of this study is to highlight important differences in characteristics and outcomes of unprovoked VTE compared to provoked VTE in pediatric patients.
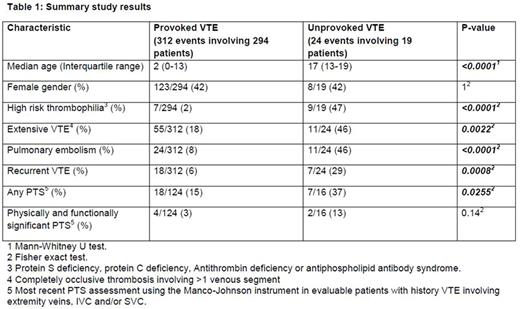
Method: We performed a retrospective analysis of a prospectively maintained institutional thrombosis database. We identified all patients with an objectively confirmed VTE at our institution over a 5-year period from 2011 to 2016. Patients were managed according to standardized institutional protocols based on published guidelines. We compared patients with unprovoked VTE to those with provoked VTE with regards to demographics, prevalence of high risk thrombophilia (defined as inherited deficiency of antithrombin, protein C, or protein S, or antiphospholipid antibody syndrome), frequency of extensive VTE (defined as completely occlusive thrombosis involving >1 venous segment), frequency of pulmonary embolism (PE), frequency of recurrent VTE and frequency of post-thrombotic syndrome (PTS) assessed using the Manco-Johnson instrument in evaluable patients with history of VTE involving extremity veins, inferior vena cava, and/or superior vena cava. Data was compared using the Mann-Whitney U test or Fisher exact test as appropriate. Two-tailed p value less than 0.05 was considered statistically significant.
Results: See Table 1 for a summary of the results. A total of 313 patients developed 336 VTE events at our institution during the study period. Of 336 VTE events, 24 (7%) were unprovoked events affecting 19 patients. Patients with unprovoked VTE were significantly older compared to patients with provoked VTE while gender distribution was similar between the 2 groups. The prevalence of high risk thrombophilia was significantly higher in patients with unprovoked VTE. Similarly, the frequencies of extensive VTE, PE and recurrent VTE were significantly higher in patients with unprovoked VTE. The frequency of physically and functionally significant PTS was not significantly different between the two groups. However, the frequency of PTS of any severity was significantly higher in patients with unprovoked VTE.
Conclusion: Our study indicates that pediatric patients with unprovoked VTE represent a distinct patient population that appears to be at high risk for poor outcomes. Multicenter, prospective studies are needed to confirm our results and for developing optimal evidence-based risk stratified treatment approaches.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal